Your Trusted Vascular Medicine Surgeon in Jacksonville, FL
Our Vascular Medicine Surgery Specialist in Jacksonville, FL
has Years of Experience as an Interventional Radiologist
Venous disease is prevalent across the United States. If you, like many other Americans, suffer from venous disease, be sure to work with a venous disease doctor that you can trust in Jacksonville, FL. At Ponte Vedra Vein Institute, we want you to be happy and healthy in your own skin.
Your Venous Disease Specialists
At Ponte Vedra Vein Institute, we understand that seeking treatment for vascular conditions can be overwhelming and intimidating. That's why we're proud to offer the expertise of our highly trained vascular medicine surgeon to patients in Jacksonville, FL.
Vascular medicine is the branch of medicine focused on the diagnosis and treatment of vascular diseases, which affect the body's blood vessels, including arteries and veins. Our vascular medicine surgeon with years of experience as an interventional radiologist utilizes cutting-edge technologies and techniques to provide the highest level of care to each patient, ensuring the best possible outcome.
Whether you're dealing with varicose veins, spider veins, or other vascular issues, our surgeon will work with you to develop a personalized treatment plan that meets your specific needs. At Ponte Vedra Vein Institute, we're committed to delivering compassionate care, putting your comfort and well-being at the forefront of everything we do.
Read on to learn more about the other services we offer our patients.
Continue reading this page to learn vital information about venous disease and the specific medical issues that can arise from it, such as varicose veins and blood clots. Call us today at 904-280-0600 or fill out our online contact form to schedule your free consultation.
Approximately 27 percent of American adults have some type of venous disease in their legs, according to the Vascular Disease Foundation. This equates to an estimated 20 to 25 million people in the U.S. who suffer from one of many serious venous diseases and disorders, and the numbers are even higher among older Americans. At Ponte Vedra Vein Institute, we specialize in diagnosing and treating the entire spectrum of venous disease.
Causes
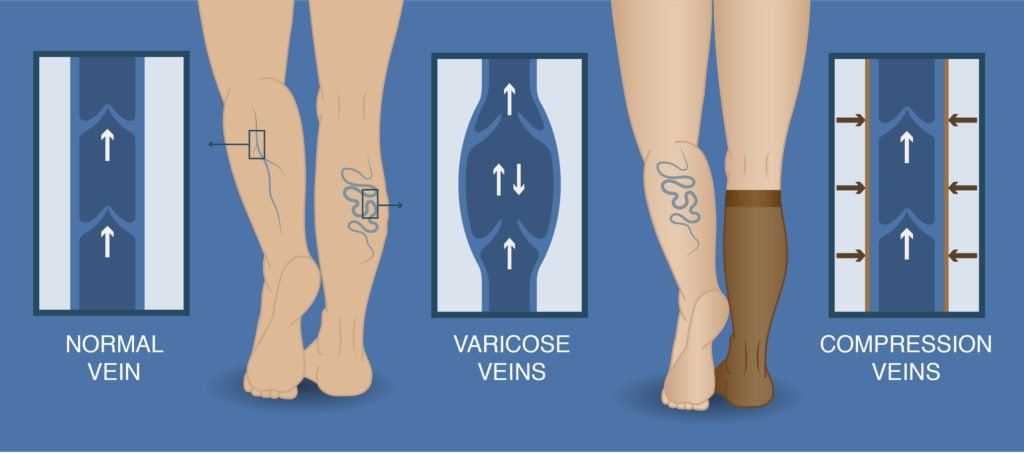
Venous disease results when veins’ walls and valves are damaged or weak and do not function properly. Normally, valves in veins and muscles work together to move blood forward to the heart. Muscles contract to squeeze the blood along; when they relax, valves prevent the blood from moving backward. When a venous disorder or disease is present, valves can be too weak to perform their normal function, allowing blood to pool or flow in both directions. Venous or vascular disease is associated with a number of issues, including:
- Varicose veins
- Spider veins
- Blood clots
- Chronic venous insufficiency (CVI)
- Deep vein thrombosis (DVT)
Several factors may play a role in venous diseases, with heredity being one of the most common causes. Additional factors include aging, reduced mobility, inactivity, obesity, and leg injuries. Lifestyle choices and cumulative health can also affect vascular health.
Venous Disease used to be primarily treated by vascular surgeons with older hospital-based stripping procedures. With the advancement of technology treatments are now easy office based treatments that allow patients better results with little to no downtime. When choosing a vein doctor it is important to be educated on the different specialties of medicine which are medically indicated to treat vascular disease; to include Interventional Radiologists, Vascular Surgeons, and Interventional Cardiology. Other specialties have not received the extensive training required to fully evaluate and treat a patients; vascular needs. Interventional Radiology is a highly specialized branch of medicine that combine the power of advanced imaging ( Cat scans, MRI, and ultrasounds) these physicians are highly trained to not only read and interpret imaging but through minimally invasive procedures are able to treat conditions that were once difficult and dangerous.
Symptoms
Symptoms of venous or vascular problems in the legs include:
- Swelling or changes in the skin
- Aching, burning sensations, fatigue, itching, or feelings of heaviness
- Pain or cramping in the calves
- Leg ulcers
- Enlarged or varicose veins
Left untreated, venous disease can worsen and become more severe. Some conditions—such as deep vein thrombosis, or blood clots that can break loose and travel to the lungs—can even be life-threatening. Medical care for venous issues should be sought as soon as possible.
Chronic Venous Insufficiency
What is chronic venous insufficiency (CVI)?
When veins in the leg function properly, leg movement, such as walking, causes muscles to contract and blood to be pumped back up to the heart through a series of valves. Healthy valves maintain a normal pressure, moving blood along as they open and close. When a vein or valve is diseased, damaged, or weakened, however, blood may pool or drain backward. This may result in a number of conditions, including varicose veins. Left untreated, these conditions may lead to chronic venous insufficiency.
Symptoms of chronic venous insufficiency:
CVI shares many of the same symptoms that other conditions present, including:
- Pain that worsens when standing and improves when legs are raised
- Tingling sensations and itching in the leg
- Cramping, aching, and a sense of heaviness
- Skin changes, such as red or swollen areas
- Varicose veins
- Leg ulcers that are slow to heal
CVI risk factors and causes:
It is estimated that more than 2.5 million people suffer from chronic venous insufficiency. Some patients may suffer from this condition due to:
- A history of blood clots in the leg
- A history of CVI in the family
- Age
- A sedentary lifestyle
- Pregnancy
- Obesity
- Long periods of standing or sitting on the job
In addition, females may be more susceptible to developing CVI due to hormone levels.
Prevention measures include maintaining a healthy weight, avoiding sitting or standing for prolonged, uninterrupted periods of time, increasing daily activity, and seeking early treatment for any signs of CVI.
Diagnosing and treating CVI:
Our board-certified interventional radiologists will consult with you and discuss all of your treatment options. These include compression stockings to improve blood flow, sclerotherapy, phlebectomy, or endovenous laser ablation. Our vascular specialists are experts in using the latest minimally invasive procedures to treat chronic venous insufficiency and other vascular conditions.
Depending up the procedure that’s best for your needs, treatment time is often less than an hour, and you should be able to quickly return to your normal activities.
If you have symptoms of chronic venous insufficiency, we invite you to schedule a free vascular analysis.
Pelvic Veins
What is pelvic congestion syndrome?
Pelvic congestion syndrome (PCS) may also be referred to as pelvic venous congestion syndrome (PVCS), ovarian vein reflux, or ovarian vein and pelvic varices. The chronic pain of PCS may be caused by varicose veins in the thigh, or vaginal or buttock regions.
As with varicose veins, veins in the pelvic area may become less elastic or the valves that prevent blood from flowing backwards become weakened. This allows blood to pool and the vein to enlarge.
Unlike many varicose veins that are easily seen on the skin’s surface, the veins involved with PCS may be more difficult to detect. It’s important to seek treatment from specially trained vascular and interventional radiology specialists who can accurately diagnose PCS and recommend the most appropriate treatment.
Signs and symptoms of pelvic congestion syndrome:
When a vein’s valves are compromised or the vein is enlarged due to a loss of elasticity, patients may experience one or more of these symptoms:
- Pain or aches in the lower abdomen or pelvic area
- A sensation of fullness in the legs
- Pain that worsens when lifting or standing
- Pain that worsens as the day goes on, then lessens after a night’s sleep
- Urinary symptoms, such as worsened stress incontinence
Some pregnant women develop the condition, which can continue after pregnancy. Symptoms may also coincide with a woman’s menstrual cycle as hormone levels fluctuate.
The embolization procedure:
Catheter-directed embolization is a nonsurgical, minimally invasive procedure that helps eliminate blood flow within the vein. Tiny coils are used to stop the abnormal blood flow and relieve pain and pressure. The treatment is performed through a vein in the groin or neck, and requires only a band-aid as dressing. Patients may immediately return to their normal daily routines.
Benefits of embolization include:
- No surgical incision or stitches are needed
- The procedure is highly effective for a majority of patients
- The risk of infection is very small
- No post-procedural downtime
- Embolization is done on an outpatient basis
Ambulatory Phlebectomy
Ambulatory Phlebectomy is minimally invasive surgery to remove superficial varicose veins.
Ambulatory phlebectomy or “micro-phlebectomy” or “stab phlebectomy is a safe and effective outpatient procedure performed to remove large bulging, painful veins. This allows patients to resume their routine activities almost immediately following the procedure. The phlebectomy procedure entails complete removal of these abnormal/diseased veins in a microextraction procedure through very tiny incisions that requires no stitches.
There is minimal to no discomfort following Ambulatory Phlebectomy. Some patients may experience slight swelling and bruising following the procedure which may require mild pain relievers. Patients may stand, walk and return to work on or the day following the procedure.
Why Ambulatory Phlebectomy
- Same day, walk in-walk out
- All done within the office
- No anesthesia
- Very tiny punctures
- No down-time
- Excellent results
Procedure
- Preoperative skin markings are performed by our Vein Specialist physician.
- Local anesthesia is administered after cleaning the skin.
- Tiny incisions are made and to remove the diseased veins.
- Once the diseased veins have been removed, your leg is bandaged. No stitches required.
- Compression stocking is then placed and worn for a 48 hours
Post Procedure
- All patients are able to go home directly following the procedure.
- We have patients “walk about” for a few minutes to ensure the wrapping is comfortable
- Any pain can be managed with Ibuprofen., Tylenol or Hydrocodone
- Patients usually return to the office in two weeks for a check-up/follow-up
- Our Vein Specialist physician is on call 24/7 to respond to any post-operative need
All medical treatments are covered by insurance including Medicare.
Contact us today to schedule your FREE consultation!
Compression Therapy
Compression therapy is a simple and effective method for maintaining and increasing blood flow.
Medical compression stockings are utilized to support the venous system in the legs. They apply graduated compression; which is greatest at the ankle and diminishes as it reaches the thigh. Compression stockings “squeeze” fluids (venous blood and lymph) out of the legs and towards the heart, and are useful for decreasing mild leg swelling, slowing the progression of varicose veins and preventing deep vein thrombosis. They are generally worn throughout the day, and for extended periods of time.
Most insurance companies require a therapeutic trial of medical compression stockings (or some other conservative therapy) prior to authorizing surgical or minimally-invasive varicose vein treatment. Compression stockings are also commonly used post-operatively after vein treatments (e.g. Sclerotherapy, Radio-Frequency Ablation, Endovenous Laser Ablation, Ambulatory Phlebectomy) to aid in healing. Many types of compression hose are available such as, knee-high, thigh-high, pantyhose and maternity style.
Traditionally, patients with varicose veins were usually recommended conservative treatment options without the use of medications or surgery. Physicians would suggest lifestyle changes, such as eating less, exercising more and wearing compression stockings which only improved leg pain and further deterioration or worsening of the venous system. However, conservative treatment will not remove existing abnormal veins.
Compression Therapy
- Provides a gradient of pressure, highest at the ankle, decreasing as it moves up the leg
- Reduces reflux of blood
- Improves venous outflow
- Increases velocity of blood flow to reduce the risk of blood clots
Ask one of our team members today about the different strengths, styles and colors of compression stockings at
Ponte Vedra Vein Institute for both men and women.
All medical treatments are covered by insurance including Medicare.
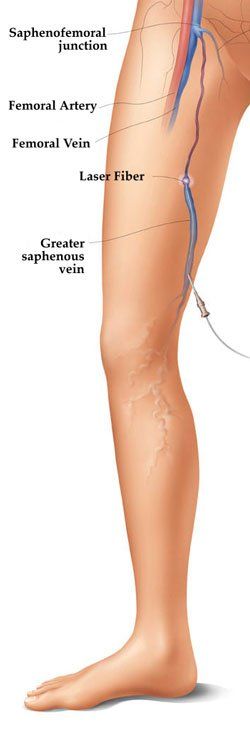
Endovenous Laser Ablation
ELA requires no sedation and uses thermal energy to break down varicose veins and ultimately disappear.
Endovenous Laser Ablation (EVLA) utilizes laser energy, which is simply a highly concentrated beam of light. Medical lasers work by delivering this light energy to the targeted tissue with extreme precision, without damaging the surrounding tissue. Lasers have proven safe and effective through years of use in all types of medical procedures, from eye surgery to dermatology. In the hands of a skilled physician, laser procedures produce far fewer complications than conventional surgery.
Initially, ultrasound is utilized to map the course of a diseased vein. Subsequently, the physician guides a thin fiber into the diseased vein, through a small incision in the skin and vein wall. The laser fiber is advanced under ultrasound guidance through the vein and appropriately positioned. The fiber delivers pulsed laser heat to the diseased vein wall, thus closing and sealing the varicosed vein, and eliminating venous reflux. The vein is treated in segments as the catheter is gradually retracted towards the incision. When the entire vein has been ablated, the blood flow is automatically rerouted through adjacent healthy veins, restoring and improving circulation and reducing swelling. Possible rare complications of endovenous laser treatment are thermal skin burns and transient numbness.
EVLA is reimbursed by Medicare and most private insurers, once proof of medical necessity has been documented and the patient has failed conservative therapy. Approved for use in the United States by the Food and Drug Administration in 2002, EVLA is performed in a physician’s office utilizing local anesthesia. Patients are encouraged to walk immediately following the procedure, and are usually able to resume their normal activities within twenty-four hours. Compression stockings are generally prescribed for one to two weeks following the procedure.
All medical treatments are covered by insurance including Medicare.
Contact us today to schedule your FREE consultation!
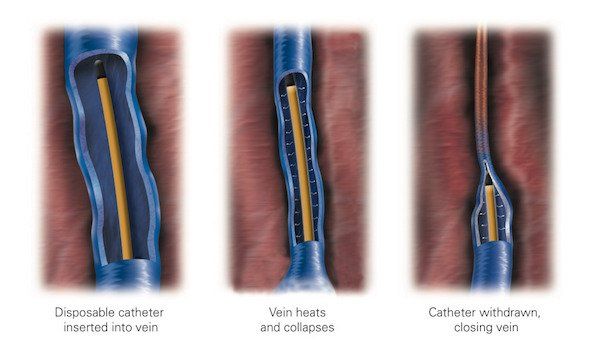
Radio-Frequency Ablation
Radiofrequency is used to create heat and cauterize the varicose veins.
Radio-frequency Ablation (RFA), also called the Closure procedure, is a minimally invasive varicose vein treatment technique that utilizes radiofrequency energy (electricity) to heat, collapse and seal targeted blood vessels.
Initially, ultrasound is utilized to map the course of the a diseased vein. Subsequently, the physician guides a catheter (thin tube) into the diseased vein, through a small incision in the skin and vein wall. The catheter is advanced under ultrasound guidance through the vein and appropriately positioned. Electricity is delivered to a heating element in 20-second pulses, heating and contracting the collagen within the walls of the vein until they shrink and permanently collapse. This process is called ablation.
The vein is treated in segments as the catheter is gradually retracted towards the incision. When the entire vein has been ablated, the blood flow is automatically rerouted through adjacent healthy veins, restoring and improving circulation and reducing swelling. The ablated vein becomes scar tissue and is absorbed by the body. Possible rare complications of endovenous radiofrequency ablation are thermal skin burns and transient numbness.
RFA is reimbursed by Medicare and most private insurers, once proof of medical necessity has been documented and the patient has failed conservative therapy. Approved for use in the United States by the Food and Drug Administration in 1999, RFA is performed in a physician’s office utilizing local anesthesia. Patients are encouraged to walk immediately following the procedure, and are usually able to resume their normal activities within twenty-four hours. Compression stockings are generally prescribed for one to two weeks following the procedure.
RFA offers a variety of benefits including:
- Relief of symptoms
- Minimally invasive, nonsurgical procedure
- Same day, outpatient procedure
- Minimal downtime
- Minimal or no scarring
All medical treatments are covered by insurance including Medicare.
Contact us today to schedule your FREE consultation!
Sclerotherapy for Spider Veins
Sclerotherapy is typically the treatment of choice for smaller varicose or spider veins.
Sclerotherapy is often used to treat visible spider veins and small varicose veins near the surface of the skin. A painless sclerosant is injected into the veins, causing them to shrink, occlude and eventually disappear. Although two to five treatments are often needed, the results are long-lasting.
Advantages of Sclerotherapy
- No downtime
- Less likely to stain skin
- Long-lasting results
- Fewer allergic reactions
- No scarring
Contact us today to schedule your FREE consultation!
Ultrasound-Guided Sclerotherapy
Here we use ultrasound technology to create a detailed map of the treatment area.
Foam or Liquid Sclerotherapy
Ultrasound-Guided Sclerotherapy UGS or (Echo-Sclerotherapy) is an in-office treatment alternative to surgical stripping. Based on the clinical judgment of the physician, sclerotherapy is performed utilizing either a liquid or “foamed” sclerosant, while the vein is monitored via ultrasound. This enables the treatment of veins that are not visible because they are below the surface of the skin, and would otherwise require surgical removal. Ultrasound is utilized to guide a needle into the abnormal vein, which delivers medication that obliterates the lining of the blood vessel, thus causing it to collapse and seal shut.
Ultrasound-guided sclerotherapy is primarily used to treat large veins beneath the surface of the skin.
All medical treatments are covered by insurance including Medicare.
Contact us today to schedule your FREE consultation!
Varithena®
Varithena® does not require the use of general anesthesia, sedation, or incisions to treat varicose veins.
Learn more about how Varithena®’s advanced microfoam technology collapses veins in a non-surgical manner.
Varithena® is a minimally-invasive, non-surgical solution for treating a wide range of varicose veins that uses injectable microfoam technology. Designed to collapse unhealthy veins in a non-surgical setting, Varithena® does not require the use of general anesthesia, sedation, or incisions.
How Varithena® Works
Varithena® ‘s microfoam interacts with the vein walls to collapse them safely and effectively. As the foam is pushed out of the collapsing vein, it is then distributed throughout nearby veins — collapsing connected veins that are malfunctioning similarly, and dissolving safely into the bloodstream of healthier veins.
This way, blood flow is rerouted through healthier veins, providing you enhanced circulatory functions and immediate relief from physical pain and discomfort.
Types of Veins Treated With Varithena®
Varithena® can treat a variety of varicose veins, both above and below the knee, including:
- Veins of all sizes (including small, medium, and large diameters
- Veins previously treated by other medical methods
- Twisted veins (also called tortuous veins)
What To Expect From Your Procedure
Your physician will begin by performing an ultrasound to assess the diseased veins in your leg and map out where, specifically, they will administer the Varithena®.
Using either a catheter or direct injection, your physician will then administer Varithena®, placing mild pressure on the leg to help distribute the microfoam particles and collapse the diseased vein(s). Ultrasound technology will be used to monitor the position of the catheter throughout the procedure.
Once complete, the catheter will be removed. The site will be covered with a bandage and you will be provided with a medical compression stocking for your leg.
VenaSeal™
VenaSeal™ takes a breakthrough approach of applying a medical adhesive to close the vein.
On October 27th 2016, Dr. Megan Deacon-Casey, Interventional Radiologist at Ponte Vedra Vein Institute, performed the first VenaSeal ™ procedure in Northeast Florida to treat varicose veins.
The VenaSeal™ closure system is the only non-tumescent, non-thermal, non-sclerosant procedure that uses a proprietary medical adhesive delivered endovenously to close the vein. This unique approach eliminates the risk of nerve injury when treating the small saphenous vein, which is a risk sometimes associated with certain thermal-based procedures.1,2 Clinical studies have demonstrated that the procedure is safe and effective.1-4 The procedure is administered without the use of tumescent anesthesia, avoiding patient discomfort associated with multiple needle sticks.
All medical treatments are covered by insurance including Medicare.
What to Expect
Before the VenaSeal™ Closure Procedure:
You will have an ultrasound imaging exam of the leg that is to be treated. This exam is important for assessing the diseased superficial vein and planning the procedure.
During the Procedure:
- You may feel some minor pain or stinging with a needle stick to numb the site where the doctor will access your vein.
- Once the area is numb, the doctor will insert the catheter (i.e., a small hollow tube) into your leg. You may feel some pressure from the placement of the catheter.
- The catheter will be placed in specific areas along the diseased vein to deliver small amounts of the medical adhesive. You may feel some mild sensation of pulling or tugging. Ultrasound will be used during the procedure to guide and position the catheter.
- After treatment, the catheter is removed and a bandage placed over the puncture site. Compression stockings are placed on the treated leg.
After the Procedure:
The medical staff will review post-treatment instructions with you.